Pancreatic Cancer
Hoag Family Cancer Institute
949-722-6237
- About
- Diagnosis
- Early Detection Program
- Treatment Options
- Meet the Team
- Clinical Trials & Research
- FAQ
Every person needs a team of dedicated experts to help them beat pancreatic cancer. Hoag gives you access to subspecialized experts, the most advanced diagnostic and treatment options, and groundbreaking clinical research.
Quick Support
Clinical Trials & Research
Through innovative clinical research, Hoag physicians explore the efficacy of new drugs, therapies, medical devices and clinical and surgical methods – ensuring you have access to the most advanced treatments available.
Supportive Resources
Hoag is the top choice for cancer care in Orange County, with cancer survival rates that continually exceed national averages. Our dedicated, world-class teams are wholly focused on helping you survive cancer, heal and move forward with your life.

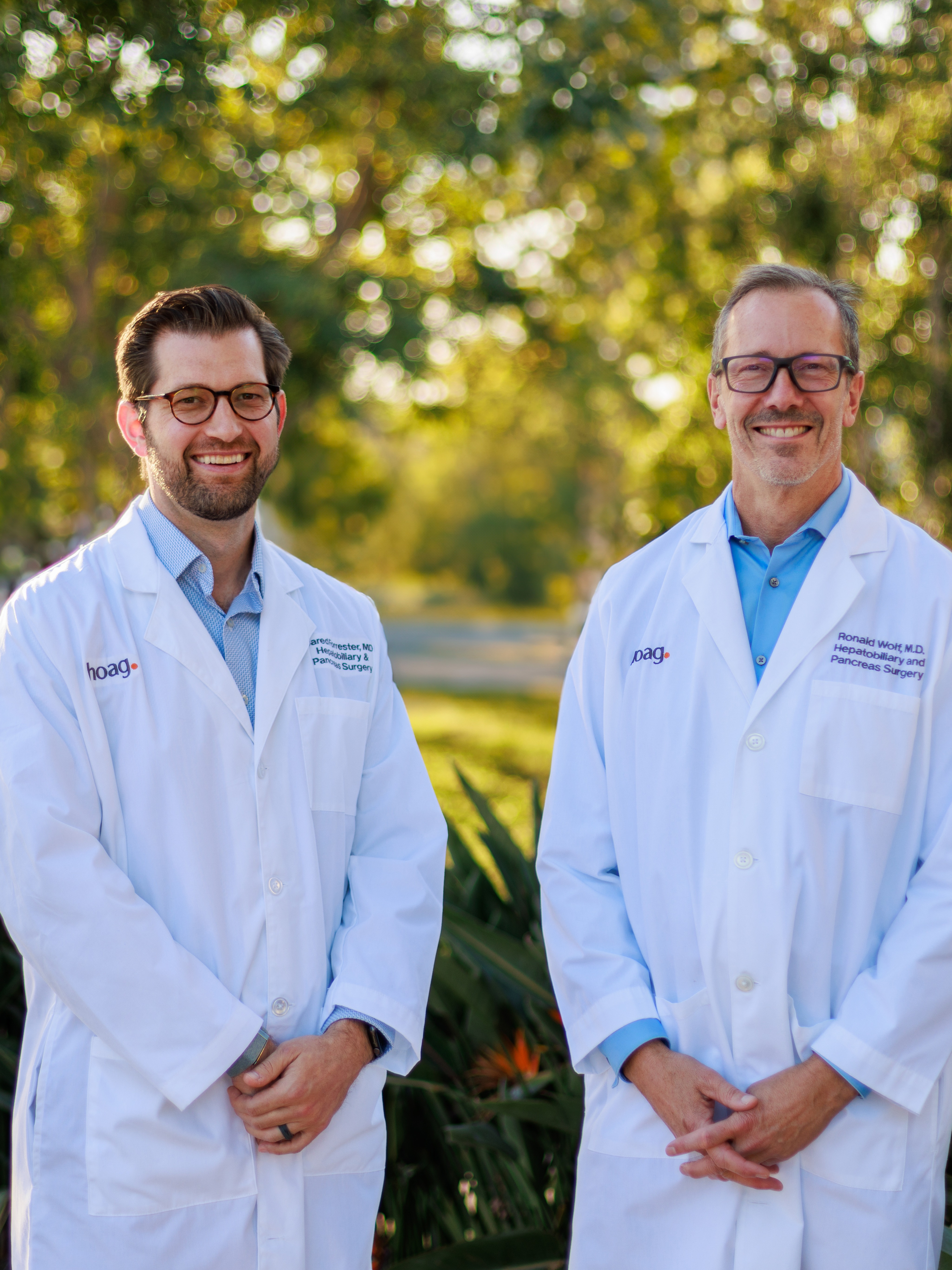
World-Class Hepatobiliary Surgeons – Right Here in OC
Medical Oncologists Subspecialty Trained in Your Condition

Personalized Treatment

Advanced Interventional GI

Pancreatic Cyst Surveillance Program

Hoag Family Cancer Institute Locations
Hoag Memorial Hospital Presbyterian
- 1 Hoag Drive, Building #41
- Newport Beach, CA 92663
Begin Your Journey
1
Find the Right Provider
Get care from medical providers that fit your needs in a location near you.
Find a provider2
Explore Cancer Resources
Find information made to guide and support you on your journey.
See all resources3
Get in touch
Didn’t see what you’re looking for? Reach out and we’ll make sure you get what you need.
Contact usExpert Diagnosis is Key
Comprehensive evaluation with accurate diagnosis is the foundation for achieving successful outcomes. That’s why it’s important to seek care from a center that provides academic level care from a multidisciplinary, specialized team of hepatobiliary and pancreatic experts experienced in the accurate diagnosis of pancreatic cancer, as well as other complex gastrointestinal diseases.
Beginning with a thorough evaluation that includes a comprehensive physical exam, personal medical history review and state-of-the-art diagnostic workup, Hoag’s multidisciplinary team of board-certified, fellowship trained pancreatic experts carefully evaluate and pinpoint the nature of the cancer, so the most appropriate personalized treatment options can be employed.
Hoag’s state-of-the-art diagnostic technologies provide our team with the latest modalities in the accurate diagnosis of pancreatic cancer and other disorders. Some of the progressive imaging studies that may be utilized include:
Volume Rendering Computed Tomography (CT) is the most recent advance in CT technology. Only a few centers in Southern California have this technology, which creates highly accurate 3-D scans of the pancreas. This enables physicians to properly stage the cancer and determine whether the tumor is resectable.
Endoscopic Ultrasound (EUS) uses an ultrasound device to make images of your pancreas from inside your abdomen. The physician may also collect a sample of cells (biopsy) during EUS.
Endoscopic Retrograde Cholangiopancreatography (ERCP) uses a dye to highlight the bile ducts in the pancreas, so that an accurate image of the bile duct and pancreatic duct may be obtained. This study is performed to rule out certain diseases of the pancreas and the bile duct. The physician may also insert small tubes (called stents) into the bile duct or the pancreatic duct, if they are obstructed, to relieve the obstruction. Additionally, a tissue sample (biopsy) may be collected during ERCP.
MRCP is a modified MRI that utilizes specialized software to obtain a composite image of the pancreatic duct and the bile duct from the digital MRI images. This study provides similar information to an ERCP. However, as a diagnostic study, MRCP study is preferred to ERCP since this procedure is not invasive.
Tumor Markers are used to determine whether certain substances are being released into the blood. Tumor markers are often obtained to assess the probability of a cancer in a patient who has a lesion. While high tumor markers may indicate cancer, they are not definitive since non-cancerous conditions of the pancreas and liver can falsely elevate these tumor markers.
Diagnostic Laparoscopy is a minimally invasive surgical procedure used to examine internal organs by direct visualization. Small incisions are made in the abdominal wall, and a thin, lighted tube called a laparoscope is inserted. This procedure allows the surgeon to evaluate whether the cancer has spread outside of the pancreas prior to performing surgery. This is an important part of planning for surgery.
Biopsy is the removal of a sample of tissue for testing. This procedure is performed to definitively diagnose pancreatic cancer, and may involve other methods outside of laparoscopic biopsy, such as endoscopic ultrasound or fine-needle aspiration.
It’s important to note that proper diagnosis and staging of pancreatic cancer is critical to developing a successful treatment plan. That’s why it’s so important to seek proper evaluation and treatment from a healthcare expert experienced in the most advanced pancreatic cancer care.
Innovative Treatment for Pancreatic Cancer
When it comes to pancreatic cancer and other gastrointestinal diseases, Hoag Family Cancer Institute provides a full array of progressive treatment options. As a recognized leader and high-volume provider of innovative gastrointestinal care, Hoag’s multidisciplinary team of digestive disease experts performs some of the most advanced gastrointestinal procedures available in the nation with clinical outcomes that rival national figures.
Expert Care You Can Trust
Hoag Family Cancer Institute provides state-of-the-art, compassionate pancreatic cancer care. Hoag’s committed to accurate diagnosis, combined with progressive therapeutic options enables Hoag patients to achieve some of the highest clinical outcomes in the nation.
To schedule a comprehensive diagnostic evaluation, or a second-opinion consultation with a Hoag pancreatic cancer expert, call us at 949-764-5350.
Anita Erickson Pancreatic Cancer Early Detection Program
Pancreatic cancer is the fourth leading cause of cancer death in both men and women in the United States. In 2015, there were 49,000 new diagnoses with almost as many deaths (41,000). Early disease detection can change this.
As the first in Southern California and one of only a few centers in the U.S., Hoag Family Cancer Institute now offers a clinical research study and early detection program to assess individuals at higher risk of developing pancreatic cancer. The purpose of this program is to improve the outcomes for individuals at risk for pancreatic cancer, working to detect early stage cancer through labs, imaging and diagnostic testing, as well as genetic counseling and testing. As part of the program, individuals will also submit their de-identified information to be part of a registry, shared by similar organizations in the nation. This database will help future clinicians to better understand this complex disease and how to effectively treat and manage it.
Individuals with family members who were diagnosed with pancreatic cancer, or those with positive genetic test results in certain genes, are qualified for the program and the registry.
Hoag’s Pancreatic Cancer Early Detection Program is led by a multidisciplinary team of specialists including a geneticist, genetic counselors, gastroenterologists and GI surgeons. Together, this team supports all aspects of care, collaborating with other physician specialists, to ensure an individual’s risk is accurately assessed and treated.
This program was made possible thanks to a generous gift from the estate of Anita Erickson.
If you have any questions, please contact the Anita Erickson Pancreatic Cancer Early Detection Program at 949-764-8805.
Pancreatic Cancer: Types of Treatment
When it comes to pancreatic cancer and other gastrointestinal conditions, expert evaluation is vital to accurately diagnose pancreatic cancer and then determine the best course of treatment for the individual patient.
At Hoag, our multidisciplinary team of experts work together to thoroughly review and determine the pancreatic cancer treatment option suited to each individual patient.
The team then carefully tailors a personalized treatment plan to effectively achieve the best possible outcome for the patient. This emphasis on a collaborative, comprehensive approach to patient-centered care is why Hoag patient outcomes rank are among the nation’s best.
Once pancreatic cancer is diagnosed, important staging tests (such as diagnostic laparoscopic examination) are performed to determine if the cancer has spread, and if so, to what extent. The type of treatment recommended depends upon the stage of the cancer and may include options such as:
Pancreatic Cancer Surgery
Pancreatic cancer treatment options depends on the type of tumor and where in the pancreas the tumor is located.
Innovative surgical treatment is offered for patients with an adenocarcinoma of the pancreas since this tumor is associated with a poor outcome if not completely eradicated by surgery. However, in patients with less aggressive cancers, surgical treatment, including minimally invasive approaches, may be indicated in selected cases. Hoag’s philosophy is to always emphasize organ preservation whenever possible.
When it comes to advanced surgical care, the Hoag surgical team performs more complex pancreatic surgeries than any other surgical program in Southern California including state-of-the-art procedures that may not available at most centers. Being a high-volume pancreatic cancer surgical program enables the gastrointestinal experts at Hoag to achieve a technical skill level not all facilities can match.
Some of the advanced surgical options for treating tumors of the pancreas include:
The Whipple Operation involves resection (removal) of the head of the pancreas, a portion of the bile duct, the gallbladder and the duodenum. Occasionally, a portion of the stomach may also be removed. The Whipple Operation is often used to treat patients with adenocarcinoma of the pancreas, although it may be recommended for some patients with benign disorders such as chronic pancreatitis and benign tumors of the head of the pancreas.
Central Pancreatectomy may be recommended for patients who have low-grade malignant or benign tumors in the neck of the pancreas. Removal of tumors in this area often requires removing a large portion of the pancreas. However, Hoag offers a highly specialized surgical procedure that removes only the tumorous portion of the neck of the pancreas, thereby preserving the head, body and tail of the pancreas.
Laparoscopic/Robotic-Assisted Pancreatectomy is a minimally invasive surgical procedure where the body and tail of the pancreas is removed along with the spleen. This procedure is most frequently performed in patients with adenocarcinoma of the pancreas. However, Hoag routinely provides laparoscopic spleen-preserving pancreatectomy for patients with cystic tumors and neuroendocrine tumors.
Duodenum Preserving Pancreatic Head Resection is offered primarily to patients with chronic pancreatitis, although the procedure may also be offered to some patients with neuroendocrine tumors who would otherwise require a Whipple Operation. In this procedure, the head of the pancreas is removed while preserving the bile duct and duodenum (the first part of the intestine). Hoag is one of the few centers in the United States to offer this innovative surgical procedure.
Enucleation of pancreatic islet cell tumors is surgical procedure that carefully removes islet cell tumors without removing any pancreatic tissue. Pancreatic islet cell tumors (also called neuroendocrine tumors) are small tumors found on the surface of the pancreas. Hoag surgeons have developed a laparoscopic technique for enucleation of pancreatic islet cell tumors, which provides a number of benefits to patients including a faster recovery and return to daily activities.
Locally Advanced Pancreatic Cancer
Locally advanced pancreatic cancer describes pancreatic cancer that involves other structures near the pancreas. The most frequently involved structure is the portal vein.
At Hoag, our expert team of hepatobiliary surgeons is experienced in advanced surgical techniques that allow the cancer to be removed with reconstruction of the portal vein utilizing an innovative vein graft procedure. In addition to the portal vein, other adjacent structures can also be removed, if necessary, and reconstructed using similar advanced surgical techniques.
It’s important to note that often patients with pancreatic cancer are told that their cancer is not resectable, or that they may not be a candidate for surgery. At Hoag, our academic-level hepatobiliary surgeons have extensive experience and training in complex pancreatic surgery, and can often resect locally advanced tumors due to their expertise, which is why it’s important to seek out a second opinion.
Non-Surgical Treatment Options
In addition to progressive surgical options, Hoag also provides the full array of innovative non-surgical options for treating pancreatic cancer, including:
Radiation therapy may be recommended before or after cancer surgery, often in combination with chemotherapy. Combination radiation therapy and chemotherapy may also be utilized in cases where a cancer cannot be treated surgically.
Chemotherapy uses drug therapy to help destroy cancer cells. Chemotherapy is often combined with radiation therapy to treat cancer that has spread beyond the pancreas to nearby organs, but not to distant regions of the body. This combination chemotherapy-radiation therapy protocol may also be used after surgery to reduce the risk that pancreatic cancer may recur. In individuals with advanced pancreatic cancer, chemotherapy may be used alone or it may be combined with targeted drug therapy.
Targeted therapy uses drugs that attack specific abnormalities within cancer cells. For example, the targeted drug erlotinib (Tarceva) blocks chemicals that signal cancer cells to grow and divide. This drug is usually combined with chemotherapy for use in people with advanced pancreatic cancer.
Clinical Trials play a significant role in gastrointestinal cancer treatment. Hoag physicians participate in a variety of clinical trials in order to bring advanced care to Hoag pancreatic cancer patients.
The Most Advanced Pancreatic Cancer Treatment Options Are Available at Hoag
When it comes to seeking out the most advanced pancreatic cancer care, there is no longer any need to travel long distances. Hoag Family Cancer Institute offers the latest in state-of-the-art diagnosis and leading-edge treatment options that may not be readily available at other centers, including resection of advanced pancreatic cancers, as well as participation in clinical trials that helps to bring advanced care to even more patients.
Perhaps the most distinguishing aspect of Hoag’s advanced treatment of pancreatic conditions is that in each and every case, treatment is always specifically tailored to the meet the unique needs of the individual patient.
Expert Care You Can Trust
Hoag Family Cancer Institute provides state-of-the-art, compassionate pancreatic cancer care. Hoag’s committed to accurate diagnosis, combined with progressive therapeutic options enables Hoag patients to achieve some of the highest clinical outcomes in the nation.
To schedule a comprehensive diagnostic evaluation, or a second-opinion consultation with a Hoag pancreatic cancer expert, call us at 949-764-5350.
Orange County's Leading Pancreatic Cancer Specialists
Pancreatic Cancer Surgeons

Ronald F. Wolf, MD
Ronald Wolf, M.D., F.A.C.S., is a board-certified surgical oncologist who specializes in treating liver, bile duct and pancreatic cancer at Hoag Family Cancer Institute. His clinical interests include pancreatic adenocarcinoma, colon and rectal cancers that have metastasized to the liver, surgical treatment for bile duct tumors and cysts and surgery for soft tissue sarcoma. Previously, Dr. Wolf served as Professor of Clinical Surgery in the Department of Surgery, Division of Hepatobiliary & Pancreas Surgery/Islet Cell Transplantation at UC Irvine School of Medicine and Long Beach Memorial Medical Center. Prior to that, he served as Medical Director of Hepatic and Pancreatic Surgery at Legacy Good Samaritan Medical Center in Portland, Oregon, and as the Medical Director of Liver and Pancreas Surgery at Providence Cancer Center, also in Portland. Dr. Wolf received his medical degree from Oregon Health & Science University in Portland, followed by an internship and two residencies in general surgery at UC Davis. He then completed a fellowship in surgical oncology at Memorial Sloan Kettering Cancer Center in New York, where he also served as a clinical research fellow. Later, he helped direct surgical resident and fellowship-level postgraduate training programs in Portland. Dr. Wolf has co-authored more than 80 clinical presentations throughout his career and is a committee member of several national organizations including the American College of Surgeons, the Society of Surgical Oncology and the AHPBA Americas Hepatopancreatobiliary Association.
Christine Chung, DO
<div> <p dir="ltr"><span>Dr. Chung's journey into medicine was profoundly shaped during college when she founded a chapter of a nonprofit organization, Global Medical Brigades. Through medical mission trips to rural Honduras, she helped provide healthcare to underserved communities—offering medical exams, surgical referrals, treating infections, and even assisting with infrastructure projects like stoves and irrigation systems. This meaningful experience sparked her commitment to serve others by helping to heal them. </span></p> <p dir="ltr"><span>Guided by her faith and a servant-leader mindset, Dr. Chung finds deep purpose in the relationships she forms with her patients, especially during their most vulnerable moments. She specializes in conditions and surgeries of the liver, pancreas, bile duct, and surrounding organs, and approaches each case with empathy, diligence, and a commitment to treating every patient as she would a member of her own family. </span></p> <p dir="ltr"><span>Dr. Chung earned her medical degree from Western University College of Osteopathic Medicine of the Pacific, and completed her general surgery residency at Swedish Medical Center. She is board certified in general surgery, and completed a Hepatopancreaticobiliary (HPB) fellowship at Virginia Mason Franciscan Health. She is passionate about providing exceptional, comprehensive, and compassionate clinical care with excellence and integrity. She has a special interest in multidisciplinary work and minimally invasive approaches in surgery. </span></p> <p dir="ltr"><span>Outside of medicine, she enjoys traveling, spending time outdoors, weightlifting, Pilates, yoga, and experiencing the arts, including the symphony and ballet performances. </span></p> </div>
Pancreatic Cancer Medical Oncologist
Carlos R. Becerra, MD
Medical Director of Cancer Research for Hoag Family Cancer Institute

Tara E. Seery, MD
<p>Tara Seery, M.D., attended University College Dublin School of Medicine followed by an internship at Mater Misericordiae Hospital as well as an internship and residency at Caritas St. Elizabeth Medical Center in Boston. She then completed fellowships in hematology/oncology at both Caritas St. Elizabeth Medical Center and University of Illinois at Chicago. Dr. Seery is board certified in Medical Oncology and Hematology.</p><p>Dr. Seery is particularly interested in GI oncology, including hepatobiliary cancers such as pancreatic, liver and bile duct cancers.</p><p>She has served as the primary investigator on several clinical research trials, co-authored numerous medical publications and abstracts, and edited multiple peer-reviewed journals. Additionally, she has given clinical presentations both across the U.S. and abroad. </p><p>Dr. Seery’s teaching experience spans the areas of medical and graduate level courses including a Hematology/Oncology Fellowship Annual Lecture Series on Pancreatic Cancer, Liver Cancer and the Management of Unresectable Hepatocellular Carcinoma at UC Irvine’s 5th Annual Gastroenterology and Hepatology Symposium. In addition, she oversaw a group of Hematology/Oncology Fellows at the University of California Irvine Outpatient Clinic.</p><p>Dr. Seery is a member of the American Society of Clinical Oncology and the American Society of Hematology.</p>
Radiation Oncologists
Molecular Imaging & Therapy Team

Gary A. Ulaner, MD
James & Pamela Muzzy Endowed Chair in Molecular Imaging and Therapy; Director, Molecular Imaging and Therapy

Ryan P. Reddy, MD
Diagnostic Radiology, Nuclear Medicine
Advanced Endoscopists
Phuong T. Nguyen, MD
Phuong T. Nguyen, M.D., is the Medical Director of Hoag Advanced Endoscopy Center and a therapeutic endoscopist in Newport Beach. She has clinical interests in interventional endoscopy, endoscopic ultrasound (EUS), gastroesophageal reflux disease (GERD), endoscopic bariatrics (weight management), gastrointestinal oncology (pancreatic tumors) and pelvic floor health. Dr. Nguyen is a nationally recognized expert in the field of gastroenterology, and she is one of Orange County’s most experienced physicians in the use of minimally invasive gastrointestinal procedures, including her expertise in the outpatient imaging procedure EUS and endoscopic interventions for the treatment of GERD and obesity. Additionally, she is the original co-founder of a nonprofit organization, Association of Women Endoscopists (AWE), which promotes education in the field of gastroenterology, both locally and internationally. Dr. Nguyen graduated from the David Geffen School of Medicine at the University of California, Los Angeles, and completed an internal medicine internship and residency at the University of Pennsylvania/Graduate Hospital. She completed a fellowship in gastroenterology and therapeutic endoscopy at the University of California, Irvine. She is board-certified by the American Board of Internal Medicine in gastroenterology and speaks Vietnamese.

Ravi J. Kankotia, MD
Dr. Kankotia is a board-certified gastroenterologist at the Hoag Digestive Health Institute. His focus is in advanced endoscopic procedures, and his clinical interests include pancreaticobiliary disease, tissue resection, Barrett’s esophagus, and bariatrics. Other services offered include luminal stenting, radiofrequency ablation, endoscopic mucosal resection, esophageal pH monitoring (Bravo), liver biopsy, portal pressure measurement, and endoscopic suturing. He strives to provide his patients and their families with personalized care plans that help each patient reach their health goals. At the Hoag Digestive Health Institute, Dr. Kankotia works with a team of digestive health experts to provide a comprehensive approach to wellness. Dr. Kankotia earned his medical degree at the Keck School of Medicine of the University of Southern California in Los Angeles. He completed internal medicine residency and gastroenterology fellowship at University of Southern California/LAC+USC Medical Center. He then completed an additional fellowship in advanced endoscopy at the University of Michigan in Ann Arbor, where he developed expertise in ERCP (endoscopic retrograde cholangiopancreatography), diagnostic and therapeutic EUS (endoscopic ultrasound), and other techniques while garnering experience managing complex cases. Dr. Kankotia is a current member of the American College of Gastroenterology, American Gastroenterological Association, and American Society for Gastrointestinal Endoscopy. Additionally, he has contributed to several publications on topics such as gastric cancer, biliary disease, pancreatic cysts, and luminal strictures.

Paul J. Korc, MD
Paul J. Korc, M.D. serves as medical director of the Hoag GI Lab and is a board-certified gastroenterologist with fellowship training in advanced endoscopic procedures. After completing his residency and fellowship at USC, he went on to spend a year at Indiana University, one of the nation’s top programs for biliary and pancreatic disorders. There, he received training in endoscopic retrograde cholangiopancreatography (ERCP) and endoscopic ultrasound (EUS), gaining extensive experience in the management of complex cases. Dr. Korc’s expertise also includes removal of large polyps and early stage cancers of the gastrointestinal tract, using endoscopic mucosal resection (EMR) and endoscopic submucosal dissection (ESD). He spent time in Seoul, Korea learning ESD, a cutting-edge technique in which pre-cancerous lesions and superficial cancers are removed en bloc (in one piece), avoiding the need for surgery. Additionally, Dr. Korc performs peroral endoscopic myotomy (POEM), a specialized procedure that restores the ability to eat and drink for people with achalasia, an esophageal motility disorder. Dr. Korc brings to Hoag his expertise in these procedures, some of which are available at only a handful of medical centers in Southern California. Dr. Korc offers patients compassionate, personalized care along with the very best advances in endoscopic treatment.
Pathology
Pancreatic Cancer Nurse Navigator
Hoag's Precision Medicine Program
Hoag’s Precision Medicine Program combines genomics and genetics to diagnose, treat, and prevent diseases. Using the latest advances in genomic technologies, targeted therapies and research, our precision medicine program brings together a multidisciplinary team, including a robust genetic counseling group of experts, to provide patients with the latest in innovation and technology.
Hoag’s Molecular Imaging & Therapy (MIT) Program
Hoag’s Molecular Imaging & Therapy (MIT) Program has been recognized as one of only 48 Radiopharmaceutical Therapy Centers of Excellence in the world. Through this program, Hoag is helping pioneer the most sensitive imaging methods to date to advance research and applications of molecular imaging and therapy in the treatment of cancer patients. These trials are expected to play a significant role in cancer detection, individualized treatment and drug development. The future of cancer detection and therapy is offered today at Hoag.
Hoag Family Cancer Institute Genetic Counselors
Hoag Family Cancer Institute provides a dedicated team of genetic counselors that offer hereditary cancer assessment, offering risk assessment and genetic cancer testing to those with a personal or family history of cancer.
Hoag Family Cancer Institute Social Workers
Being diagnosed with cancer can feel overwhelming at times. Many patients and their families need help with coping and can benefit from supportive counseling. Oncology Clinical Social Workers are available to provide emotional and practical support during all stages of cancer including diagnosis, treatment and post-treatment survivorship.
Hoag Family Cancer Institute Dietitians
Hoag Family Cancer Institute dietitians work closely with patients’ physicians, nurses, therapists, and social workers to ensure complete care.
Clinical Trials for Pancreas
Hoag is committed to leading the way in state-of-the-art technologies and advanced treatment options. Part of this commitment includes clinical research with the goal of helping patients live longer, healthier lives. Through carefully planned clinical trials, researchers evaluate the safety and effectiveness of new ways to diagnose, treat and prevent diseases or conditions. Treatments studied in clinical trials might be new drugs or new combinations of drugs, new surgical procedures or devices, or new ways to use existing treatments. View clinical trials for pancreatic cancer here.
World-Class Cancer Treatment. Right here in OC.
Hoag is the top choice for cancer care in Orange County, with cancer survival rates that continually exceed national averages. Our dedicated, world-class teams are wholly focused on helping you survive cancer, heal and move forward with your life.
Do I Have Pancreatic Cancer?
Pancreatic cancer begins in the pancreas, a small, tapered organ about six inches long that sits behind the stomach. When healthy, the pancreas has two different types of tissue with two different functions. Exocrine tissue, which makes up the majority of the pancreas, creates enzymes that help the body digest food. Endocrine tissue in the pancreas creates and releases hormones called insulin and glucagon that help the body maintain healthy levels of blood sugar.
When changes in the pancreas cause cells to mutate and replicate out of control, this can cause pancreatic cancer. According to the American Cancer Society , most pancreatic cancers begin in exocrine tissue, with around 95 percent classified as adenocarcinomas. Also known as ductal carcinoma, this form of the disease usually originates in the ducts that carry enzymes inside the pancreas.
Rarer forms of pancreatic cancer include:
- Colloid Carcinoma
- Adenosquamous Carcinoma
- Squamous Cell Carcinoma
Pancreatic cancer is particularly dangerous in that it often presents few or no symptoms until after it has spread to other tissues inside the body. Some symptoms of pancreatic cancer can include:
- Itchy skin or rash
- Pain that extends from the abdomen to the back
- Loss of appetite
- Blood clots
- Unexplained fatigue
- Unexplained or unintentional weight loss
- Bowel obstruction, due to a tumor pressing against the intestine and blocking the flow of waste through the body
- Jaundice, which is a yellowing of the eyes and skin
- Dark-colored urine
- Light-colored stools
- Sudden onset of diabetes, or recent difficulty controlling diabetes with medication and diet
While the vast majority of shoulder pain is related to strains, muscle pulls, arthritis or the wear-and-tear of aging, there are rare cases where pain in the shoulder or under the shoulder blade was found to be a symptom of pancreatic cancer, including this case from the American Journal of Gastroenterology and this case from 2013 . In these cases, pancreatic cancer shoulder pain is due to tumors spreading from the pancreas, then pressing on nearby nerves as they grow. These instances are rare, and most shoulder pain isn’t related to pancreatic cancer. However, if you experience unexplained pain in your shoulder that is hindering your ability to function, see your doctor.
Though the root cause of pancreatic cancer is still unknown, there are a number of factors that are believed to increase your risk of developing pancreatic cancer. These include:
- A history of pancreatitis, which is a painful inflammation of the pancreas.
- Diabetes, particularly Type 2
- A family history of pancreatic cancer
- Being older, as pancreatic cancer is usually diagnosed in people over age 65.
- A family history of certain genetic conditions, including Lynch syndrome, Familial Atypical Mole-Malignant Melanoma Syndrome (FAMMMS), mutation of the BRCA2 gene, Peutz-Jeghers Syndrome and Familial Melanoma and Hereditary colon cancer.
- Excessive alcohol use
- Smoking
- Eating a high fat diet
- Obesity
Ways to reduce your risk of developing pancreatic cancer may include:
- Avoid being overweight by eating a healthy diet and getting regular exercise to avoid being overweight. Here at Hoag, we offer help with weight management to help reduce this risk and others that come with being overweight.
- Don’t smoke
- Use alcohol in moderation
- Avoid Type 2 diabetes by cutting sugar and eating a healthy diet